
Hysterectomy in Los Angeles for Fibroids
Surgical Removal Of The Uterus
What is a hysterectomy?
A hysterectomy surgery for fibroids is a major procedure most commonly performed by a gynecologist in a hospital setting. The goal of the procedure is to partially or completely remove the uterus. By having a surgical removal of the uterus, fibroids within the uterus (the source of symptoms) are also removed. A hysterectomy can be total or partial (removal of the uterine body while leaving the cervix intact), but regardless of the type of hysterectomy, the patient will no longer be able to become pregnant.
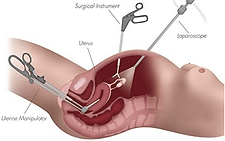
There exist a number of techniques through which hysterectomy can be performed, including abdominal hysterectomy, vaginal hysterectomy, and a number of laparoscopic techniques. See the cystectomy diagram below. Abdominal hysterectomies are the most common form of the procedure and typically require the longest recovery time. For an abdominal hysterectomy, the uterus is removed through a horizontal incision on the lower abdomen, sometimes called a “bikini cut”. The operation requires general anesthesia, and most patients will spend 3 days in the hospital. Recovery generally takes 6 weeks, assuming there are no surgical complications. The patient will retain a 4-inch scar at the incision site near the “bikini line”. Hysterectomy surgery comes with a number of risks, including blood loss and infection, all of which should be discussed with your physician.¹
A laparoscopic hysterectomy also has the objective of surgically removing the uterus, but the approach is through four smaller (1 centimeter) incisions rather than one larger one. If the fibroids or uterus are larger than average, a laparoscopic hysterectomy may not be recommended due to the need to remove substantial matter through the small incisions. In this procedure, the abdomen is filled with carbon dioxide gas in order to create a working and viewing space. The laparoscope is a thin instrument used to visualize the ovaries, fallopian tubes, and uterus. Other thin surgical instruments are then used to surgically cut and remove some or all of the uterus (along with the fibroids). At the end of the procedure, the gas is released, and the skin incisions are closed. Most patients will spend one night in the hospital followed by 2-4 weeks recovering at home. The patient will have four small scars where the incisions were made.¹

Abdominal hysterectomy
(removal through the abdomen)

Vaginal hysterectomy
(removal through the vagina)
Example laparoscopic hysterectomy technique
How does hysterectomy work?
As the fibroids are contained within the uterus, surgical removal of the uterus also removes the source of the symptoms. Bleeding symptoms are directly attributable to the uterus, and the pain symptoms associated with uterine fibroids are typically due to the fibroids coming in contact with nearby anatomy (bladder, nerves, etc.). Removal of the uterus has shown to reliably alleviate these symptoms.
Is hysterectomy clinically proven?
Hysterectomy surgery has been proven to significantly reduce symptoms due to uterine fibroids. However, the procedure is classified as a major surgery and carries a 3% risk of major complications.²
How does hysterectomy compare to other treatment options?
Hysterectomy is certainly the most invasive of treatment options for uterine fibroids, and the most serious type of surgery one can undergo for uterine fibroids. As with any surgery, there are benefits and risks that should be discussed with your hysterectomy doctor. One benefit of hysterectomy is that once the uterus is removed, fibroids can no longer recur. Another benefit is that removal of the organ ensures that in the very rare event that the mass or masses were cancerous (it's estimated that between 1 in 2000 and 1 in 340 cases are cancerous), then the tumor(s) and surrounding tissue are removed all at once. Patients who undergo a hysterectomy are less likely to need a repeat procedure than patients who choose UFE or myomectomy.³
Risks of a hysterectomy include blood loss and the possible need for transfusion, infection during the surgery or at the incision site, among other major and minor surgical complications. Evidence suggests women who undergo a hysterectomy surgery are more likely to require a blood transfusion than women undergoing UFE.² They also take longer to recover, resume regular activities, and return to work, relative to those who choose UFE.³ Weaker evidence suggests a higher rate of major complications during hysterectomy as compared with UFE, but this point is debated.³⁻⁴
Learn more about the pros and cons of a hysterectomy.
Is hysterectomy right for me?
Several factors should be discussed with your physician before deciding on hysterectomy. These include, but are not limited to: the patient’s age, the size and number of fibroids, the patient’s desire to remain fertile, and desired time to return to normal activities. If you're considering fibroid treatment, we recommend that you familiarize yourself with all of your options.
Hysterectomy Los Angeles
If you are interested in discussing a hysterectomy in Los Angeles with a hysterectomy doctor - contact the Fibroid Specialists of University Vascular today!
References
[1] Shiber, L.-D. J., & Pasic, R. (2018). Choosing the Correct Hysterectomy Technique. In I. Alkatout & L. Mettler (Eds.), Hysterectomy: A Comprehensive Surgical Approach (pp. 143–147). Cham: Springer International Publishing.
[2] Garry R, Fountain J, Mason S, Hawe J, Napp V, Abbott J, et al. The eVALuate study: two parallel randomised trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ 2004;328(7432):129.
[3] Gupta JK, Sinha A, Lumsden MA, Hickey M. Uterine artery embolization for symptomatic uterine fibroids. Cochrane Database of Systematic Reviews 2014, Issue 12. Art. No.: CD005073.
[4] Younas K, Hadoura E, Majoko F, Bunkheila A. A review of evidence-based management of uterine fibroids. The Obstetrician & Gynaecologist 2016;18:33–42.